Sydney woman Lois Harris has become one of the first Australians to report promising results from an experimental cancer treatment, after being diagnosed with a rare and incurable cancer more than a decade ago.
Lois, 73, was told in 2012 she had neuroendocrine cancer, a rare illness that often spreads before it is discovered.
Standard chemotherapy was unlikely to help, and other treatments risked damaging her kidneys, so she received injections to manage symptoms and slow the cancer instead.
“It has spread everywhere — my neck, ribs, liver and small intestine. I’ve never been led to believe they could cure it,” she told Insight.
Her condition remained stable for years, but in 2023 a tumour in her liver became more active, bringing symptoms including dizziness, diarrhoea, fatigue and a painful rash.
With limited options left, she turned to a treatment she had helped research for SBS documentary, Cancer Killers.
The film was about a new drug known as EnGeneIC Dream Vector (EDV), developed by two Australian scientists. With her disease progressing, she asked whether she could try the therapy.
She travelled to Singapore and received EDV through a cannula twice a week for two seven-week cycles, with each session lasting about three hours.
After treatment, she said her scans showed improvement.
“The tumour in my liver that was acting up has decreased by about eight millimetres and I’m in stable disease again. That’s a great result for me,” she said. She also reported no side-effects.
“I just went home and carried on with life… It’s the complete opposite of conventional chemo.”
A patient in Los Angeles, Anne Jonas, who had end-stage pancreatic cancer, also credited EDV with saving her life, two and a half years after she was told she only had weeks to live.
“I’m here having breakfast with you… I’m going to be a grandma,” she said.
Anne is the first known person in the world who has made a complete recovery from end-stage pancreatic cancer.
EDV works by entering cancer cells and destroying them from the inside while leaving healthy cells alone. This means patients avoid common chemotherapy side-effects such as nausea and hair loss.
It is also cheaper to produce than many modern cancer drugs, raising hopes it could be widely accessible.
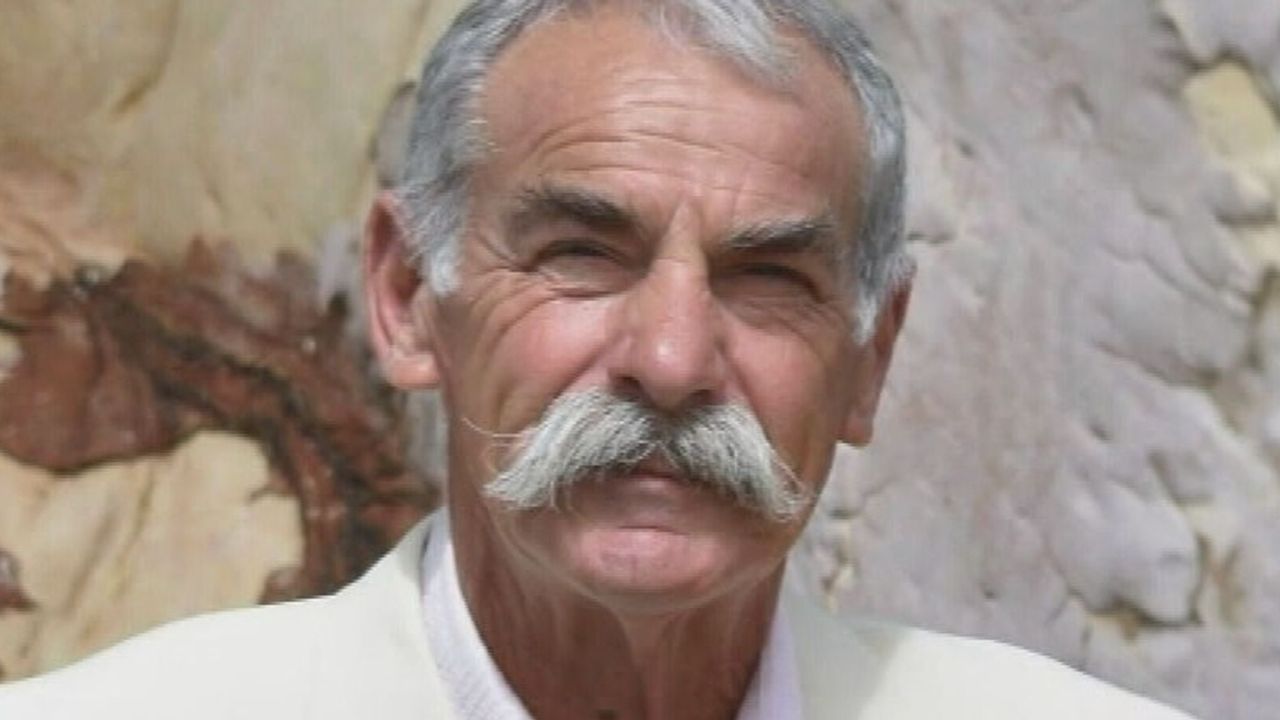
The drug was created by former CSIRO researchers Dr Jennifer MacDiarmid and Dr Himanshu Brahmbhatt, who spent years developing the idea.
“Medicine takes an incredibly long time. There have been so many points where we’ve had to rebuild from scratch,” Dr Brahmbhatt said.
The treatment entered early human trials in Melbourne in 2009 and is now moving into advanced trials in Australia, Singapore and the US, countries where the Food and Drug Administration has granted it “fast-track” status to speed review.
Cancer experts say while early results are encouraging, many new treatments never make it through full testing because cancer is complex and trials take years.
“A lot of great inventions vanish before they ever get the chance to help anyone,” Dr Brahmbhatt added.
Between 3 and 5 per cent of cancer drugs that begin Phase 1 trials in the US are eventually approved.
Despite the challenges, developers remain hopeful, with Dr Brahmbhatt saying: “That is part of what makes it so exciting. Many of tomorrow’s breakthroughs will come from directions we can’t yet anticipate. That’s why it’s crucial to continue supporting discovery science.”
“We want to see people go home cancer-free. There is no price that one can put on that.”
For now, Lois says her goal is simple: time. “If I can have another 10, 12 years of good years, that’s a huge win,” she said. “It’s given me a chance to lead a normal life.”
Image: SBS